Monkeypox
Definition
Monkeypox (also: monkeypox disease) is a rare viral disease caused by the monkeypox virus. Monkeypoxviruses are related to the classic humanpoxviruses and cowpoxviruses. Until now, monkeypox has been widespread in West and Central Africa.
Natural hosts of this virus are various rodents, including monkeys as false hosts.
The disease can also be transmitted to humans (zoonosis) and triggers a feverish, smallpox-like disease, which is usually much milder than smallpox. However, more severe illnesses can also occur. A vaccination is available and reduces the risk of an outbreak or mitigates the course of the disease. Overall, the prognosis can therefore be rated as favourable. In contrast to human smallpox (Variola), which has been eradicated since 1980, monkeypox is usually much milder, the disease usually heals on its own and most people recover within a few weeks.
However, severe courses can also occur in some of those affected, especially in people with a weakened immune system or children.
Chickenpox are varicella and belong to the herpes viruses. They are caused by the varicella-zoster virus. Once in the body, they can be reactivated years later in the form of shingles (herpes zoster). Monkeypox is one of the “classic” poxviruses (Orthopox variolae).
Since May 2022, more and more cases have been registered in countries where the disease had not previously occurred, including Germany. The special thing about it is that those affected had not previously traveled to countries where the virus is endemic, as was the case with cases of illness in the past, and that many transmissions apparently took place in the context of sexual activities.
Contagion / Transmission
In the current outbreak, human-to-human transmission is observed primarily through close contact, particularly through sexual activity. The transmission occurs primarily through direct contact with the typical skin or mucous membrane changes, the so-called smallpox lesions. The virus concentrations are particularly high in the smallpox lesions. Both the vesicle contents and the scab are infectious.
The portal of entry for the virus are often small skin injuries and in particular all mucous membranes (eyes, mouth, nose, genitals, anus), and possibly also the respiratory tract. Infected people are contagious until the lesions have completely healed (usually two to four weeks). It should be noted that lesions on mucous membranes are mostly not visible from the outside.
Transmission via contaminated objects such as clothing, bed linen, towels or, in special cases, via surfaces that have been contaminated with the virus through contact with infectious scab or smallpox vesicle content of an infected person has so far been described primarily in endemic areas. So far, there is no evidence that this transmission route is of major importance in the current outbreak.
Mpox/monkeypox viruses are also detectable in throat swabs – in lower concentrations than in the skin lesions. Viruses can also get into the saliva from smallpox lesions in the mouth. Transmission by large respiratory droplets with close face-to-face contact, e.g. B. in a conversation, is therefore conceivable. Such droplet transmissions have not yet been proven without a doubt. On the other hand, transmission via exhaled aerosols over longer distances seems unlikely and so far there is no evidence of this. So far, there is no evidence that monkeypox viruses can be transmitted before the onset of symptoms.
It has not yet been conclusively clarified whether the virus can also be spread through direct sexual transmission (e.g. through contact with semen) in addition to pure skin contact, but it seems possible.
Transmission from animals to humans can also occur in endemic areas. The reservoir here is not monkeys, but presumably rodents (like humans, monkeys can also be infected as false hosts). Transmission can occur, for example, through contact with infected animals (bites, secretions and excretions, close contact, animal carcasses during hunting, contact with material contaminated with viruses) or through handling the meat of infected animals.
To reduce the risk of contracting Mpox/monkeypox, skin contact should be minimized and especially no rashes or wounds should be touched. In the case of sexual contact, the probability of transmission is significantly increased. People can lower their risk by reducing the number of sex partners. Places where little or no clothing is worn and physical contact takes place, such as darkrooms, saunas or sex clubs, also harbor an increased risk of infection. Condoms can reduce the risk of infection by preventing direct contact with changes in the mucous membrane, especially in the anus.
Persons infected with Mpox/monkeypox should refrain from any form of sex (oral, anal) as long as there is a risk of transmission. In addition, people who have been infected should use condoms during sex for eight weeks after all lesions have healed, as the virus may still be present in semen for a period of time.
In the literature, the incubation period for Mpox/monkeypox is given as 3 or 4 days (lower limit) up to a maximum of 21 days. Shorter incubation times of one to three days were also observed in the current outbreak, with a median of 7 days.
Condoms can reduce the risk of infection by preventing direct contact with changes in the mucous membrane, especially in the . There are also indications that reproductive virus can also occur in the semen. Therefore, people with Mpox/monkeypox infection should use a condom during sex for eight weeks after all lesions have healed.
However, touching skin lesions on an infected person, regardless of where they are on the body, can result in transmission if you touch them with your own skin. In this respect, condoms can reduce the risk of infection, but cannot eliminate it.
Symptoms
The symptoms of monkeypox are similar to a smallpox infection. However, they are usually much milder. After an incubation period (time from infection to the appearance of the first symptoms) of between 3 days and up to three weeks, the first symptoms of monkeypox are flu-like symptoms. This includes:
- Fever (sudden, up to 40 degrees)
- Strong headache
- Severe body aches
- Muscle aches
- Back pain
- Swollen lymph nodes
- Exhaustion (tiredness)
Other symptoms of monkeypox
- Mucosal ulcers (especially in the mouth and throat)
- Conjunctivitis
- Painful skin changes in the genital area
- Scarring
Rashes in monkeypox
The skin rashes typical of smallpox usually develop a few days after the onset of the first symptoms. The rashes usually start on the face and spread to the whole body. The rashes go through four stages:
- Macula: Skin spots and skin redness
- Papula: Nodular skin changes
- Vesicles: Formation of skin blisters filled with fluid
- Pustula: The skin blisters fill with pus, burst and fall off.
However, some people have no general symptoms of the disease. Characteristic are the sometimes very painful skin changes that go through the stages from the spot to the pustule (macula, papula, vesicle and pustula) and ultimately crust and fall off.Skin changes in monkeypox over time
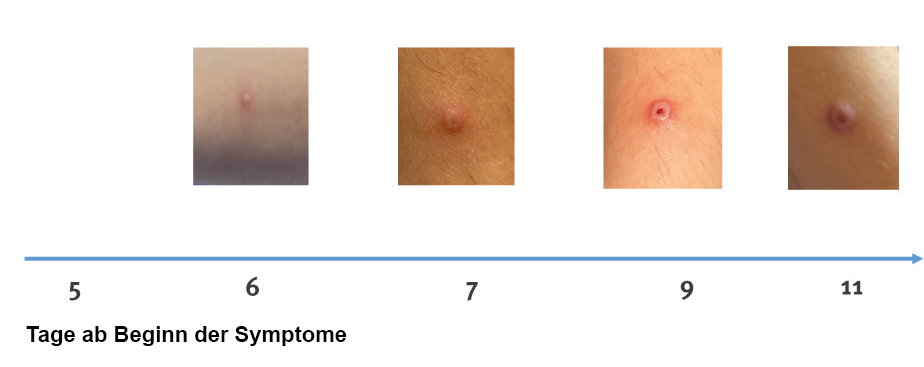
Skin changes in monkeypox over time
Source: Antinori A, 2022/Eurosurveillance
The rash can – as can often be seen in the current outbreak – appear in the genital or anal area, but also in other places such as on the hands, feet, chest or face. The skin and mucous membrane changes can also be found in the mouth and eyes. These skin changes usually last between two and four weeks and will heal on their own without treatment, although scarring may occur. Complications from bacterial superinfection of the skin lesions are possible. Manipulation of the skin lesions, such as scratching or piercing, can increase both the risk of superinfection and transmissibility.
If you suspect you have monkeypox, be sure to see a doctor to have it diagnosed.
Complications, particularly in endemic countries, include encephalitis, bacterial skin infections, dehydration, conjunctivitis, corneal and pneumonia. Serious consequences of the disease are usually disfiguring scars and permanent corneal damage, including loss of vision and death.
According to the WHO, about 3-6% of the reported cases in recent years in Central and West Africa have resulted in death. In view of the probable under-recording of cases with milder courses, the actual lethality is likely to have been lower. Case fatalities of up to 11% have been observed in children under 16 years of age infected with the more virulent Central African variant virus (clade I) in previous outbreaks. The West African variant (clade II) seems to be associated with a significantly lower case mortality.
Protection / Isolation / Duration
There is no specific vaccination against monkeypox in the EU. Due to the similarity of the virus, however, vaccines against smallpox are considered suitable for the prevention of monkeypox. The “Modified Vaccinia Virus Ankara” (MVA) is such a vaccine. It is made from weakened cowpox viruses
The antibodies against chickenpox do not work against monkeypox and vice versa. However, according to the current state of knowledge, a “real” smallpox vaccination also protects against the closely related monkeypox virus. This is due to what is known as cross-immunity.
It can be assumed that there is good basic protection against Mpox/monkeypox as early as 14 days after administration of the first vaccine dose. The 2nd vaccine dose serves in particular to prolong the duration of the vaccine protection. Immunological studies have shown that the immune protection mediated by a first vaccination decreases from 2 years after vaccination and then a second vaccine dose is required for permanent vaccination protection. The second vaccine dose should be given as soon as sufficient vaccine is available. However, it must be said that a vaccination never provides 100% protection against a disease for a variety of reasons.
But: Any vaccination is better than no vaccination and still offers good protection.
If you have been diagnosed with monkeypox, home isolation may be recommended or mandated by the authorities. This depends on the localization of the skin or mucous membrane lesions (lesions that cannot be covered) or if general or respiratory symptoms occur.
Isolation lasts until scabs and scabs heal or fall off, but at least 21 days. Condom use for 8 weeks after the end of isolation is recommended.
The Robert Koch Institute (RKI) has published a flyer for patients and household members (status: February 13, 2023). Just click on the link below (Text in German language).
https://www.rki.de/DE/Content/InfAZ/A/Affenpocken/ Isolation.pdf?__blob=publicationFile
We hope that this report has given you a brief overview of monkeypox. This report does not claim to be complete and does not represent medical advice. If you have any questions, please contact a doctor or a specialist advice center, such as the AIDS-Hilfe.